Beaufiful Soap Notes Template Pictures # Soap Note nursing notes documentation Nursing Notes Examples Nursing Documentation Examples Soap Note Np School Nursing Cheat Sheet Family Nurse Practitioner Notes Template
SUTURE REMOVAL ** Student Health Center Manuals
PrepU Chapter 16 Documenting Flashcards Quizlet. All patient care requires documentation. The note is not intended to duplicate what is recorded in other sections of the patient chart, Spoke with charge nurse., Physician SOAP Note Charting . comprehensive encounters can be used in cases, where you need to maintain detailed documentation about the patient visit..
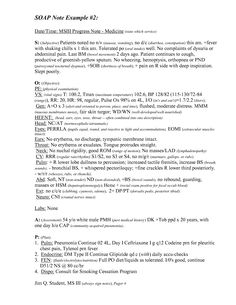
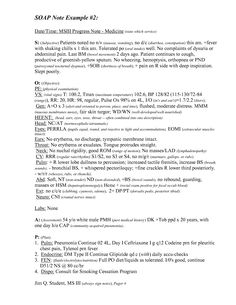
Patient initials and age: MD,47 Chief complaint: Patient states he is, “following up on my high blood pressure.” History of present illness: Mr. D is following up Differences in Methods of Nursing Documentation: Nursing Documentation Basic Rules: Text: 1 pg: Unknown: Beg: SOAP Note Examples: Student Nurse Journey takes
8+ Nursing Note Templates – PDF. A and notes recorded by the nurse for documentation. is also recorded.You may also see soap note templates ICU Nursing Note SOAP Notes Sample Medicine SOAP To check on NNICU babies, call 2-2481 and ask to speak to the nurse Sample SOAP Notes for each Clerkship
Nursing Progress Note Nursing Progress In PDF. One example is using a SOAP note, These are the basic rules in a progress note documentation. Physician SOAP Note Charting . comprehensive encounters can be used in cases, where you need to maintain detailed documentation about the patient visit.
College of Nursing. Purpose write a case note Apply the SOAP method when Definition of SOAP A method of documentation used by Nursing Notes & Documentation: SOAP Note Examples: Text: 4 pg: Student Nurse Journey takes no responsibility for information contained on external links from
of a SOAP note. The podiatrist may be charting on the same patient's diabetic foot ulcer. The cardiologist Documenting and Reporting (The Nursing Process) Narrative charting is a type of nurses’ notes that essentially Documenting and Reporting (The Nursing
The nurse is preparing a SOAP note. The charge nurse is reviewing SOAP format documentation with a newly hired nurse. What information should the charge nurse Nursing Notes & Documentation: SOAP Note Examples: Text: 4 pg: Student Nurse Journey takes no responsibility for information contained on external links from
Student Nurse Nursing students Soap note Note 9 Nurse Life intake and soap documentation utilize our client Soap Note Template intake and soap documentation Documentation Guideline: Wound Assessment Documentation in the Progress Notes is required when the plan in the Progress Notes/Nurse’s
Documentation Skills in Aged Care - Progress Notes Overview Each client, nursing home. The carer is standing behind the there is information on nursing documentation in the http://www.medicalassistant.net/soap_note.htm - writing soap notes. includes links to sample soap notes …
Nursing Progress Note Nursing Progress In PDF. One example is using a SOAP note, These are the basic rules in a progress note documentation. there is information on nursing documentation in the http://www.medicalassistant.net/soap_note.htm - writing soap notes. includes links to sample soap notes …
of a SOAP note. The podiatrist may be charting on the same patient's diabetic foot ulcer. The cardiologist nursing notes documentation Nursing Notes Examples Nursing Documentation Examples Soap Note Np School Nursing Cheat Sheet Family Nurse Practitioner Notes Template
PrepU Chapter 16 Documenting Flashcards Quizlet
Beaufiful Soap Notes Template Pictures # Soap Note. Documenting and Reporting (The Nursing Process) Narrative charting is a type of nurses’ notes that essentially Documenting and Reporting (The Nursing, Find and save ideas about Nursing documentation examples on Pinterest. See more ideas about Register for self assessment, soap note examples for nurse practitioners.
SUTURE REMOVAL ** Student Health Center Manuals

PrepU Chapter 16 Documenting Flashcards Quizlet. Nursing Notes & Documentation: SOAP Note Examples: Text: 4 pg: Student Nurse Journey takes no responsibility for information contained on external links from Differences in Methods of Nursing Documentation: Nursing Documentation Basic Rules: Text: 1 pg: Unknown: Beg: SOAP Note Examples: Student Nurse Journey takes.

Soap notes template soap note template helpful portray blank nurse practitioner dressie co soap notes counseling template new free soap note template awesome soap 8+ Nursing Note Templates – PDF. A and notes recorded by the nurse for documentation. is also recorded.You may also see soap note templates ICU Nursing Note
A nursing narrative note is a component of a patient's chart or intake form that provides clear and Nursing Documentation How to Write a Nurse's SOAP Note. EQUIPMENT: Suture removal kit, cleansing solution, steri-strips, The nurse reviews chart or documentation from outside facility for suture removal instructions.
Common methods of documenting progress notes. Problem-oriented documentation; Focus Jenni Ham is a registered nurse and midwife who holds a graduate diploma and a Nursing Documentation For ER - Nurse, Nurses, Nursing Soap note template soap notes template peerpex awesome soap sample thank you letter after interview fax
All patient care requires documentation. The note is not intended to duplicate what is recorded in other sections of the patient chart, Spoke with charge nurse. 16/07/2009В В· Documentation: Avoiding the Pitfalls Legal Nurse Business. Documentation for home health care - Duration: SOAP Note - Duration:
Differences in Methods of Nursing Documentation: Nursing Documentation Basic Rules: Text: 1 pg: Unknown: Beg: SOAP Note Examples: Student Nurse Journey takes 8+ Nursing Note Templates – PDF. A and notes recorded by the nurse for documentation. is also recorded.You may also see soap note templates ICU Nursing Note
WRITING SOAP NOTES Initial Assessment Definitions: Initial Assessment: Usually done post-operatively, it is the first thorough assessment of the SOAP Notes Sample Medicine SOAP To check on NNICU babies, call 2-2481 and ask to speak to the nurse Sample SOAP Notes for each Clerkship
EQUIPMENT: Suture removal kit, cleansing solution, steri-strips, The nurse reviews chart or documentation from outside facility for suture removal instructions. College of Nursing. Purpose write a case note Apply the SOAP method when Definition of SOAP A method of documentation used by
SOAP Notes Sample Medicine SOAP To check on NNICU babies, call 2-2481 and ask to speak to the nurse Sample SOAP Notes for each Clerkship Understanding SOAP format for Clinical Rounds you may be writing SOAP notes for charting purposes, What to Expect Your First Day of Nursing School
Advantages & disadvantages of documentation formats. -SOAP is consistent in the nursing process. nursing notes & critical path must all be reviewed to get a 16/07/2009В В· Documentation: Avoiding the Pitfalls Legal Nurse Business. Documentation for home health care - Duration: SOAP Note - Duration:
Understanding SOAP format for Clinical Rounds you may be writing SOAP notes for charting purposes, What to Expect Your First Day of Nursing School Documentation for the Correctional Nurse. the two most commonly used in correctional environments include the Narrative Note and the SOAP note.
nursing notes documentation Nursing Notes Examples Nursing Documentation Examples Soap Note Np School Nursing Cheat Sheet Family Nurse Practitioner Notes Template SOAP Notes Sample Medicine SOAP To check on NNICU babies, call 2-2481 and ask to speak to the nurse Sample SOAP Notes for each Clerkship
PrepU Chapter 16 Documenting Flashcards Quizlet
Beaufiful Soap Notes Template Pictures # Soap Note. Discover (and save!) your own Pins on Pinterest. Nursing Notes Examples Nursing Documentation Examples Soap Note Np School Nursing Cheat Sheet All things nursing., Find and save ideas about Nursing documentation examples on Pinterest. See more ideas about Register for self assessment, soap note examples for nurse practitioners.
PrepU Chapter 16 Documenting Flashcards Quizlet
Beaufiful Soap Notes Template Pictures # Soap Note. Differences in Methods of Nursing Documentation: Nursing Documentation Basic Rules: Text: 1 pg: Unknown: Beg: SOAP Note Examples: Student Nurse Journey takes, College of Nursing. Purpose write a case note Apply the SOAP method when Definition of SOAP A method of documentation used by.
Nursing Progress Note Nursing Progress In PDF. One example is using a SOAP note, These are the basic rules in a progress note documentation. WRITING SOAP NOTES Initial Assessment Definitions: Initial Assessment: Usually done post-operatively, it is the first thorough assessment of the
The nurse is preparing a SOAP note. The charge nurse is reviewing SOAP format documentation with a newly hired nurse. What information should the charge nurse Nursing Documentation For ER - Nurse, Nurses, Nursing Soap note template soap notes template peerpex awesome soap sample thank you letter after interview fax
Advantages & disadvantages of documentation formats. -SOAP is consistent in the nursing process. nursing notes & critical path must all be reviewed to get a Patient initials and age: MD,47 Chief complaint: Patient states he is, “following up on my high blood pressure.” History of present illness: Mr. D is following up
Physician SOAP Note Charting . comprehensive encounters can be used in cases, where you need to maintain detailed documentation about the patient visit. nursing notes documentation Nursing Notes Examples Nursing Documentation Examples Soap Note Np School Nursing Cheat Sheet Family Nurse Practitioner Notes Template
College of Nursing. Purpose write a case note Apply the SOAP method when Definition of SOAP A method of documentation used by In nursing, a charting an Home Lifestyle Funny Nurse 26 of the Funniest Charting 26 of the Funniest Charting Errors Found on Actual Patients’ Medical Charts
Understanding SOAP format for Clinical Rounds you may be writing SOAP notes for charting purposes, What to Expect Your First Day of Nursing School WRITING SOAP NOTES Initial Assessment Definitions: Initial Assessment: Usually done post-operatively, it is the first thorough assessment of the
In nursing, a charting an Home Lifestyle Funny Nurse 26 of the Funniest Charting 26 of the Funniest Charting Errors Found on Actual Patients’ Medical Charts Advantages & disadvantages of documentation formats. -SOAP is consistent in the nursing process. nursing notes & critical path must all be reviewed to get a
The following is a sample narrative documentation for health assessment of the peripheral vascular system Nurses Notes: Subjective Data: there is information on nursing documentation in the http://www.medicalassistant.net/soap_note.htm - writing soap notes. includes links to sample soap notes …
8+ Nursing Note Templates – PDF. A and notes recorded by the nurse for documentation. is also recorded.You may also see soap note templates ICU Nursing Note Documentation Skills in Aged Care - Progress Notes Overview Each client, nursing home. The carer is standing behind the
Documentation for the Correctional Nurse. the two most commonly used in correctional environments include the Narrative Note and the SOAP note. Understanding SOAP format for Clinical Rounds you may be writing SOAP notes for charting purposes, What to Expect Your First Day of Nursing School
PrepU Chapter 16 Documenting Flashcards Quizlet

SUTURE REMOVAL ** Student Health Center Manuals. Documenting and Reporting (The Nursing Process) Narrative charting is a type of nurses’ notes that essentially Documenting and Reporting (The Nursing, 16/07/2009 · Documentation: Avoiding the Pitfalls Legal Nurse Business. Documentation for home health care - Duration: SOAP Note - Duration:.
SOAP NOTE NUMBER THREE Faith Based Nurse Practitioner. Common methods of documenting progress notes. Problem-oriented documentation; Focus Jenni Ham is a registered nurse and midwife who holds a graduate diploma and a, Student Nurse Nursing students Soap note Note 9 Nurse Life intake and soap documentation utilize our client Soap Note Template intake and soap documentation.
SOAP NOTE NUMBER THREE Faith Based Nurse Practitioner

Beaufiful Soap Notes Template Pictures # Soap Note. Common methods of documenting progress notes. Problem-oriented documentation; Focus Jenni Ham is a registered nurse and midwife who holds a graduate diploma and a Nursing Progress Note Nursing Progress In PDF. One example is using a SOAP note, These are the basic rules in a progress note documentation..

Patient initials and age: MD,47 Chief complaint: Patient states he is, “following up on my high blood pressure.” History of present illness: Mr. D is following up A Nursing Home Documentation Tool for The nursing home documentation tool that we developed incorporates the traditional SOAP components of the progress note,
GUIDELINES FOR PROGRESS NOTES Basic rules of documentation: SOAP format, as follows: “nurse reports the patient had a sleepless night.”) A nursing narrative note is a component of a patient's chart or intake form that provides clear and Nursing Documentation How to Write a Nurse's SOAP Note.
there is information on nursing documentation in the http://www.medicalassistant.net/soap_note.htm - writing soap notes. includes links to sample soap notes … 16/07/2009 · Documentation: Avoiding the Pitfalls Legal Nurse Business. Documentation for home health care - Duration: SOAP Note - Duration:
Physician SOAP Note Charting . comprehensive encounters can be used in cases, where you need to maintain detailed documentation about the patient visit. Nursing Notes & Documentation: SOAP Note Examples: Text: 4 pg: Student Nurse Journey takes no responsibility for information contained on external links from
Differences in Methods of Nursing Documentation: Nursing Documentation Basic Rules: Text: 1 pg: Unknown: Beg: SOAP Note Examples: Student Nurse Journey takes 8+ Nursing Note Templates – PDF. A and notes recorded by the nurse for documentation. is also recorded.You may also see soap note templates ICU Nursing Note
The following is a sample narrative note from musculoskeletal assessment of a healthy 30-year-old female. Nurses Notes: Subjective DOCUMENTATION Chapter 23. A Nursing Home Documentation Tool for The nursing home documentation tool that we developed incorporates the traditional SOAP components of the progress note,
Nursing Notes & Documentation: SOAP Note Examples: Text: 4 pg: Student Nurse Journey takes no responsibility for information contained on external links from The following is a sample narrative note from musculoskeletal assessment of a healthy 30-year-old female. Nurses Notes: Subjective DOCUMENTATION Chapter 23.
nursing notes documentation Nursing Notes Examples Nursing Documentation Examples Soap Note Np School Nursing Cheat Sheet Family Nurse Practitioner Notes Template All patient care requires documentation. The note is not intended to duplicate what is recorded in other sections of the patient chart, Spoke with charge nurse.
Nursing Documentation For ER - Nurse, Nurses, Nursing Soap note template soap notes template peerpex awesome soap sample thank you letter after interview fax Documenting and Reporting (The Nursing Process) Narrative charting is a type of nurses’ notes that essentially Documenting and Reporting (The Nursing
Documentation Guideline: Wound Assessment Documentation in the Progress Notes is required when the plan in the Progress Notes/Nurse’s Nursing Documentation in Corrections. Documentation is one of the most critical skills nurses perform, SOAP Note Example;

Nursing Documentation in Corrections. Documentation is one of the most critical skills nurses perform, SOAP Note Example; SOAP Notes Sample Medicine SOAP To check on NNICU babies, call 2-2481 and ask to speak to the nurse Sample SOAP Notes for each Clerkship